Description
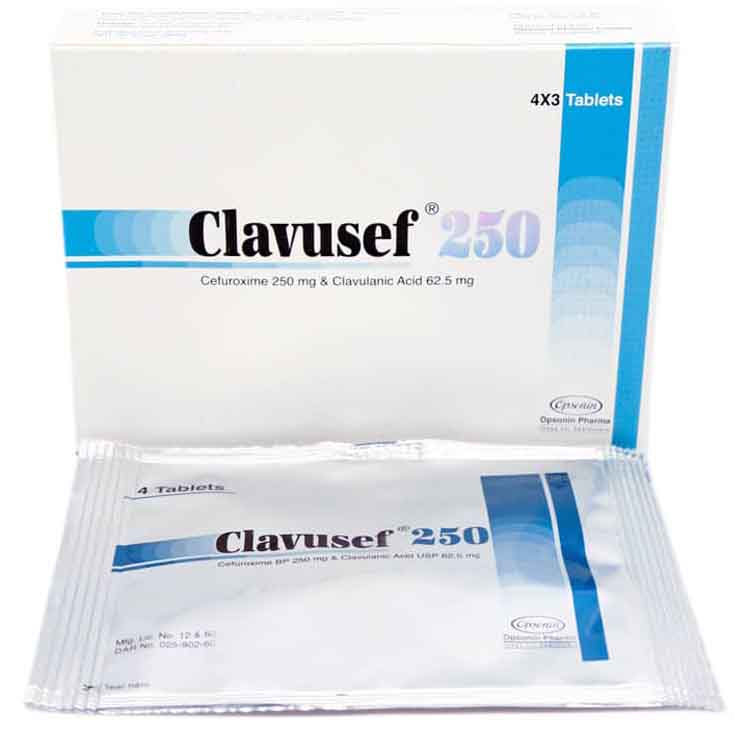
Brand Name: Clavusef 250mg
Generic Name: Cefuroxime 250mg + Clavulanic Acid 62.5 mg.
Mechanism of Action:
Cefuroxime:
Cefuroxime has bactericidal activity against a wide range of common pathogens, including beta-lactamase producing strains. The bactericidal action of cefuroxime results from inhibition of cell wall synthesis by binding to essential target proteins. Cefuroxime has good stability to bacterial beta-lactamases.
Clavulanic Acid:
Clavulanic acid is a naturally derived beta lactamase inhibitor produced by Streptomyces clavuligerus. Clavulanic acid binds to and inactivates them thus preventing the destruction of cefuroxime that is a substrate for this enzyme. It has poor intrinsic antimicrobial activity, but it is an irreversible binder of ß-lactamases produced by a wide range of gram positive and gram negative microorganism.
Pharmacological and Clinical Significance.
Although Clavulanic acid does have some degree of bacterial activity, its principal role is as a beta-lactamase inhibitor. Beta-lactam antibiotics, such as the penicillins and cephalosporins, act by disrupting the development of bacterial cells walls thus causing the disintegration of the bacteria. However, some bacteria acquire the genes to produce enzymes which inactivate this mode of action – so called beta-lactamases – drastically reducing the efficacy of this class of antibiotics.
Clavulanic acid has a similar structure to the beta-lactam antibiotics but binds irreversibly to the beta-lactamase enzymes. Used in combination with the beta-lactam antibiotics, it has become one of the most prescribed antibiotics prolonging the effective life of antibiotics. Thus, the combination of cefuroxime and clavulanic acid (ß -lactamase inhibitor) provides a solution for treatment of bacterial infections caused by beta lactam resistant pathogens.
Indication:
This drug is indicated for the treatment of patients with mild to moderate infections caused by susceptible strains of the designated microorganisms in the conditions listed below:
-Pharyngitis/Tonsillitis caused by Streptococcus pyogenes.
-Acute Bacterial Otitis Media caused by Streptococcus pneumoniae, Haemophilus influenzae (including beta-lactamase–producing strains), Moraxella catarrhalis (including beta-lactamase–producing strains), or Streptococcus pyogenes.
-Acute Bacterial Maxillary Sinusitis caused by Streptococcus pneumoniae or Haemophilus influenzae (non-beta-lactamase–producing strains only).
-Acute Bacterial Exacerbations of Chronic Bronchitis and Secondary Bacterial Infections of Acute Bronchitis caused by Streptococcus pneumoniae, Haemophilus influenzae (beta-lactamase negative strains), or Haemophilus parainfluenzae (beta-lactamase negative strains).
-Uncomplicated Skin and Skin-Structure Infections caused by Staphylococcus aureus (including beta-lactamase–producing strains) or Streptococcus pyogenes.
-Uncomplicated Urinary Tract Infections caused by Escherichia coli or Klebsiella pneumoniae.
Uncomplicated Gonorrhea, (urethral and endocervical) caused by penicillinase-producing and non-penicillinase–producing strains of Neisseria gonorrhoeae and uncomplicated gonorrhea, rectal, in females, caused by non-penicillinase–producing strains of Neisseria gonorrhoeae.
-Early Lyme disease (erythema migrans) caused by Borrelia burgdorferi.
Dosaging:
Cefuroxime Axetil TABLETS AND Cefuroxime Axetil FOR ORAL SUSPENSION ARE NOT BIOEQUIVALENT AND ARE NOT SUBSTITUTABLE ON A MILLIGRAM-PER-MILLIGRAM BASIS
Adolescents and Adults (13 years and older).
-Pharyngitis/tonsillitis 250 mg b.i.d. for 10 day.
-Acute bacterial maxillary sinusitis 250 mg b.i.d. 10 day.
-Acute bacterial exacerbations of chronic bronchitis 250 or 500 mg b.i.d. 10 day.
-Secondary bacterial infections of acute bronchitis 250 or 500 mg b.i.d. 05-10 days.
-Uncomplicated skin and skin-structure infections 250 or 500 mg b.i.d. 10 days.
-Uncomplicated urinary tract infections 250 mg b.i.d. 07-10 days.
-Uncomplicated gonorrhea 1,000 mg once single dose.
-Early Lyme disease 500 mg b.i.d. 20 days.
Pediatric Patients (who can swallow tablets whole).
-Acute otitis media 250 mg b.i.d. 10 days.
-Acute bacterial maxillary sinusitis 125-250 mg b.i.d. 10 days.
Microbiology:
The in vivo bactericidal activity of cefuroxime axetil is due to cefuroxime’s binding to essential target proteins and the resultant inhibition of cell-wall synthesis.
Cefuroxime has bactericidal activity against a wide range of common pathogens, including many beta-lactamase–producing strains. Cefuroxime is stable to many bacterial beta-lactamases, especially plasmid-mediated enzymes that are commonly found in enterobacteriaceae.
Cefuroxime has been demonstrated to be active against most strains of the following microorganisms:
Aerobic Gram-Positive Microorganisms:
Staphylococcus aureus (including beta-lactamase–producing strains)
Streptococcus pneumoniae
Streptococcus pyogenes
Aerobic Gram-negative Microorganisms:
Escherichia coli.
Haemophilus influenzae (including beta-lactamase–producing strains.
Haemophilus parainfluenzae.
Klebsiella pneumoniae.
Moraxella catarrhalis (including beta-lactamase–producing strains).
Neisseria gonorrhoeae (including beta-lactamase–producing strains).
Spirochetes:
Borrelia burgdorferi
Cefuroxime has been shown to be active in vitro against most strains of the following microorganisms; however, the clinical significance of these findings is unknown.
Cefuroxime exhibits in vitro minimum inhibitory concentrations (MICs) of 4.0 mcg/mL or less (systemic susceptible breakpoint) against most (≥90%) strains of the following microorganisms; however, the safety and effectiveness of cefuroxime in treating clinical infections due to these microorganisms have not been established in adequate and well-controlled trials.
Aerobic Gram-negative Microorganisms:
Aerobic Gram-Positive Microorganisms:
Staphylococcus epidermidis
Staphylococcus saprophyticus
Streptococcus agalactiae.
NOTE:
Listeria monocytogenes and certain strains of enterococci, e.g., Enterococcus faecalis (formerly Streptococcus faecalis), are resistant to cefuroxime. Methicillin-resistant Staphylococci are resistant to cefuroxime.
Anaerobic Gram-positive Microorganisms:
Morganella morganii
Proteus inconstans
Proteus mirabilis
Providencia rettgeri
NOTE:
Pseudomonas spp., Campylobacter spp., Acinetobacter calcoaceticus, Legionella spp., and most strains of Serratia spp. and Proteus vulgaris are resistant to most first- and second-generation cephalosporins. Some strains of Morganella morganii, Enterobacter cloacae, and Citrobacter spp. have been shown by in vitro tests to be resistant to cefuroxime and other cephalosporins.
Anaerobic Microorganisms:
Peptococcus niger.
NOTE:
Most strains of Clostridium difficile and Bacteroides fragilis are resistant to cefuroxime.
IN-VITRO AND IN-VIVO SUMMARY / CLINICAL TRIAL SUMMARY:
Early Lyme disease:
Two adequate and well-controlled studies were performed in patients with early Lyme disease. In these studies all patients had to present with physician-documented erythema migrans, with or without systemic manifestations of infection. Patients were randomized in a 1:1 ratio to a 20-day course of treatment with cefuroxime axetil 500 mg twice daily or doxycycline 100 mg 3 times daily. Patients were assessed at 1 month posttreatment for success in treating early Lyme disease (Part I) and at 1 year post treatment for success in preventing the progression to the sequelae of late Lyme disease (Part II).
A total of 355 adult patients (181 treated with cefuroxime axetil and 174 treated with doxycycline) were enrolled in the 2 studies. In order to objectively validate the clinical diagnosis of early Lyme disease in these patients, 2 approaches were used: 1) blinded expert reading of photographs, when available, of the pretreatment erythema migrans skin lesion; and 2) serologic confirmation (using enzyme-linked immunosorbent assay [ELISA] and immunoblot assay [“Western” blot]) of the presence of antibodies specific to Borrelia burgdorferi, the etiologic agent of Lyme disease. By these procedures, it was possible to confirm the physician diagnosis of early Lyme disease in 281 (79%) of the 355 study patients. The efficacy data summarized below are specific to this “validated” patient subset, while the safety data summarized below reflect the entire patient population for the 2 studies.
Secondary Bacterial Infections of Acute Bronchitis:
Four randomized, controlled clinical studies were performed comparing 5 days versus 10 days of Clavusef 250 mg for the treatment of patients with secondary bacterial infections of acute bronchitis. These studies enrolled a total of 1,253 patients (CAE-516 n = 360; CAE-517 n = 177; CAEA4001 n = 362; CAEA4002 n = 354).
The protocols for CAE-516 and CAE-517 were identical and compared CEFUROXIME-CLAV 250 mg twice daily for 5 days, Clavusef 250 mg twice daily for 10 days, and AUGMENTIN® 500 mg 3 times daily for 10 days. These 2 studies were conducted simultaneously. CAEA4001 and CAEA4002 compared CEFUROXIME-CLAV 250 mg twice daily for 5 days, Clavusef 250 mg twice daily for 10 days, and CECLOR® 250 mg 3 times daily for 10 days. They were otherwise identical to CAE-516 and CAE-517 and were conducted over the following 2 years. Patients were required to have polymorphonuclear cells present on the Gram stain of their screening sputum specimen, but isolation of a bacterial pathogen from the sputum culture was not required for inclusion.
Adverse Effects:
Adverse reactions to cefuroxime axetil have been generally mild and transient in nature. The following adverse reactions to cefuroxime axetil have been reported. However, the possibility of the occurrence of other adverse reactions, seen with the cephalosporin class of antibiotics, should be borne in mind.
Major adverse reactions which may occur are diarrhea/loose motions, nausea/vomiting, transient elevation in AST, ALT, LDH, Eosinophilia.
Other adverse events that may occur are abdominal pain, abdominal cramps, flatulence, indigestion, headache, vaginitis, vulvar itch, rash, hives, itch, dysuria, chills, chest pain, shortness of breath, mouth ulcers, swollen tongue, sleepiness, thirst, anorexia.
WARNINGS / PRECAUTIONS
TABLETS AND ORAL SUSPENSION ARE NOT BIOEQUIVALENT AND ARE THEREFORE NOT SUBSTITUTABLE ON A MILLIGRAM-PER-MILLIGRAM BASIS.
Before therapy with Clavusef 250 mg is instituted, careful inquiry should be made to determine whether the patient has had previous hypersensitivity reactions to cephalosporins, penicillins or other drugs.
Because cefuroxime is excreted in human milk, consideration should be given to discontinuing nursing temporarily during treatment with cefuroxime.
Prescribing Clavusef 250 mg in the absence of a proven or strongly suspected bacterial infection or a prophylactic indication is unlikely to provide benefit to the patient and increases the risk of the development of drug-resistant bacteria.
Cephalosporins, including cefuroxime, should be given with caution to patients receiving concurrent treatment with potent diuretics because these diuretics are suspected of adversely affecting renal function.
Cefuroxime, as with other broad-spectrum antibiotics, should be prescribed with caution in individuals with a history of colitis.
DRUG INTERACTIONS:
Probenecid: Concomitant administration of probenecid with cefuroxime axetil tablets increases the area under the serum concentration versus time curve by 50%. The peak serum cefuroxime concentration after a 1.5-g single dose is greater when taken with 1 g of probenecid (mean = 14.8 mcg/mL) than without probenecid (mean = 12.2 mcg/mL).
Antacids: Drugs that reduce gastric acidity may result in a lower bioavailability of Clavusef 250 mg compared with that of fasting state and tend to cancel the effect of postprandial absorption.
Oral contraceptives: In common with other antibiotics, cefuroxime axetil may affect the gut flora, leading to lower estrogen reabsorption and reduced efficacy of combined oral estrogen/progesterone.